We normally get scared when we see swollen, red, itchy skin…but inflammation is a good thing. It serves as a warning and helps fight the trigger.
The inflammation process
The inflammation process is a vital part of the body’s immune response to injury, infection, or tissue damage. It involves a complex series of events that aim to protect the body, remove harmful stimuli, and initiate the healing process. Here is a simplified description of the inflammation process:
- Trigger and Recognition: Allergens trigger histamine release and inflammation. Allergens may be various factors, including pathogens (bacteria or viruses), physical injury, chemicals, or autoimmune reactions. The immune system recognizes these triggers as foreign or harmful substances.
- Gates open (vasodilation and increased permeability): In response to the trigger, local blood vessels in the affected area widen (vasodilation), allowing more blood to flow. This increased blood flow causes redness and warmth in the area. Blood vessel walls also become more permeable, allowing fluid, proteins, and immune cells to move from the bloodstream into the surrounding tissue. This is dune to allow the “troops” to wage war against the trigger.
- Send in the “troops” (immune cell activation): The open gates allows the “troops” (white blood cells) to migrate to the inflamed “war zone”. Neutrophils are usually the first cells to arrive, followed by other types of immune cells, such as macrophages and lymphocytes. These cells play critical roles in fighting infection, clearing debris, and initiating tissue repair.
- Troop’s communication (release of chemical mediators): Immune cells release various chemical mediators, including histamines, cytokines, and prostaglandins. These mediators help regulate the immune response, attract more immune cells to the site, and contribute to the characteristic symptoms of inflammation, such as pain, swelling, and heat. The better our cells are at communicating with each other, the faster the war is resolved.
- Clean up the mess (phagocytosis): Pacman-like immune cells (Phagocytes such as neutrophils and macrophages) engulf and digest the trigger, foreign substances, pathogens, and cellular debris in a process called phagocytosis. This helps eliminate the source of injury or infection.
- Tissue Repair and Healing: As the inflammation subsides, the body initiates the process of tissue repair and regeneration. Fibroblasts produce collagen, which helps rebuild damaged tissue. New blood vessels form to supply nutrients and oxygen to the healing area.
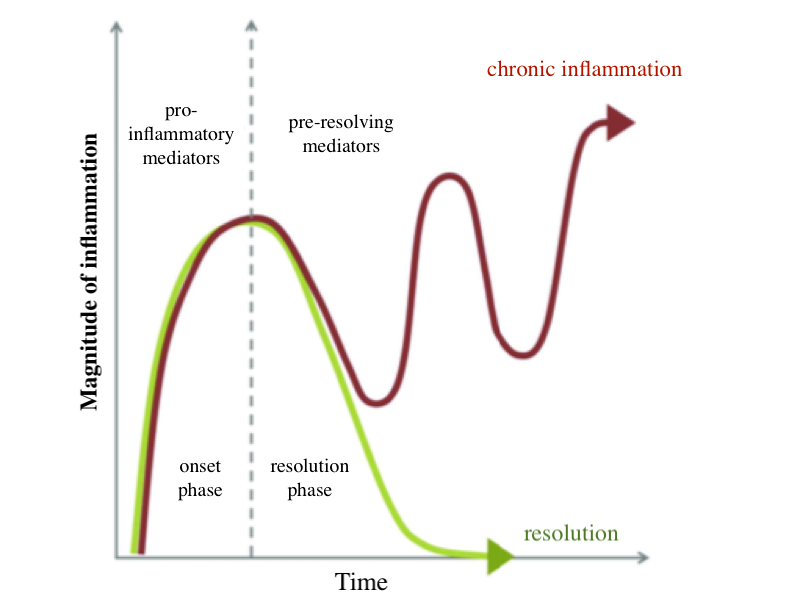
- Resolution: Inflammation gradually resolves as the triggering factors are eliminated, and the healing process progresses. In cases where the inflammation is chronic or unresolved, it can lead to tissue damage and ongoing health issues.
The best way to deal with inflammation is to help the body run its course and get to resolution as fast as possible.
When inflammation turns bad
Managing inflammation appropriately is crucial for maintaining overall health and well-being.
Inflammation becomes a problem when it cannot reach resolution. This lead to chronic inflammation which can contribute to various diseases, such as rheumatoid arthritis, asthma, inflammatory bowel disease, etc.
Resolving inflammation
Rather than symptomatic relief A better way to solve inflammation from the root cause. This entails understanding what the trigger is, understanding if it can be eliminated, understanding what we can do to make our body stronger and able to fight the trigger quickly, and understanding what we can do to support the whole inflammation process to get to resolution fastest.

References
- Chen, L., Deng, H., Cui, H., Fang, J., Zuo, Z., Deng, J., Li, Y., Wang, X., & Zhao, L. (2017). Inflammatory responses and inflammation-associated diseases in organs. Oncotarget, 9(6), 7204–7218. https://doi.org/10.18632/oncotarget.23208
- Hannoodee, S., & Nasuruddin, D. N. (2022). Acute Inflammatory Response. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK556083/


